Infarction
Myocardial Infarction Triad
Injury
(means acute or recent)
ST Depression
ST Depression
The ST segment may become depressed under certain circumstances or conditions.
During an angina attack, the ST segment may be temporarily depressed.
A subendocardial infarction, an infarct that does not extend through the full thickness of the left ventricular wall, will depress the ST segment.
Positive Stress Test
When a patient with narrowed coronaries exercises, the myocardium demands more blood flow than its arteries can deliver. A stress or exercise test will record depression of the ST segment on EKG when such a patient is exercised.
Digitalis
Digitalis can cause depression of the ST segment, however it has a unique, unforgettable appearance.
Digitalis causes a gradual downward curve of the ST segment, to give it the appearance of Salvador Dali's mustache. Notice that the lowest portion of the ST segment is depressed below the baseline.
Digitalis produces a unique, gradual downward curve of the ST segment; this is the classical "digitalis effect".
To identify the classical pattern of digitalis effect, you should observe a lead with no demonstrable S wave. The downward portion of the R wave gradually thickens as it curves down into the ST segment, which is usually depressed. The downward limb of the R wave has a gentle, curving slope that gradually blends into the depressed ST segment. Look for it the next time you have a patient on a digitalis preparation.
Subendocardial Infarction
Subendocardial infarction causes flat depression of the ST segment; however, any significant ST depression (in leads where the QRS is upright) indicates compromised coronary blood flow until proven otherwise.
Subendocardial infarction (often referred to as subendocardial injury) is identified by flat ST segment depression, which may be either horizontal or down sloping.
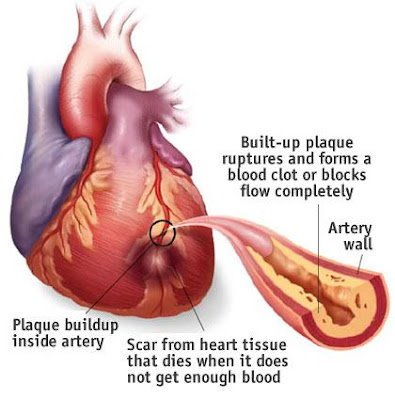
Subendocardial infarction, a type of "non Q wave infarction" involves only a small area of myocardium just beneath the endocardial lining. Classical myocardial infarction is said to be transmural; that is, the full thickness of the left ventricular wall is damaged in the infarcted area. Even though subendocardial infarction involves only a small area of the myocardium, it must be respected as a true MI that requires appropriate care. A subendocardial MI may enlarge or extend and become more life threatening.
Any patient with acute ST depression or elevation, particularly if it persists, should have an immediate, complete workup including cardiac enzymes.
Credit: Dale Dubin-RapidInterpreatation Of EKG