Type Of Cardiac Rhythm Management Devices
Many cardiac devices are designed
to help control irregular heartbeats in people with heart rhythm disorders.
These irregularities are caused by problems with the heart’s electrical system,
which signals the heart to contract and pump blood throughout the body.
At King Fahd Armed Forces
Hospital, Jeddah, our cardiac electrophysiologists implant and monitor devices
that either help the heart’s electrical system function properly or measure
heart rhythm. These devices will help us to solve a problem with heart rhythm
either bradyarrhythmias or tachyarrhtyhmias. These devices include pacemakers,
implantable cardioverter defibrillators, or ICDs, and implanted heart rhythm
monitors called loop recorders.
Pacemaker
A pacemaker is a small device
that’s implanted under the skin of the chest. It produces electrical pulses to
keep the heart beating at a normal rate. A pacemaker helps manage heart rhythm
disorders, such as bradycardia, when the heart beats too slowly, or an
arrhythmia, when the heart beats irregularly.
The size of two half-dollars
pressed together, a pacemaker contains a small computer and a battery that are
connected to one or two flexible, insulated wires called leads, which extend
from the device inside the chest to the heart.
A pacemaker is implanted in the
chest, beneath the collarbone during a procedure that requires local anesthesia
and sedation. The surgery typically takes less than an hour to complete and
usually requires an overnight stay in the hospital.
You can most likely return to
your usual activities the day after pacemaker implantation, but your doctor may
restrict some activities for two weeks. Restrictions include avoiding lifting
anything heavier than 10 pounds and not engaging in exercises such as swimming,
golf, or tennis that strain the affected side.
Two weeks after the procedure,
your doctor examines the implantation site and checks to see how well the
pacemaker is working by using a wand that transmits information stored in the
device’s generator to a computer. This includes information about the
pacemaker’s battery life, the condition of the lead or leads, and any
arrhythmias experienced since the pacemaker was implanted. The battery
typically lasts 7 to 13 years.
Every six months, you visit Pacemaker
Clinic, so your cardiovascular technologist
or electrophysiologist doctor can retrieve and analyze the information stored
on the pacemaker. Sometimes, this information can be transmitted from home via
a telephone line, cellular network, or the internet. This scheduled remote
monitoring allows for more frequent checkups while reducing the need for office
visits to once a year.
Ongoing monitoring helps your
doctor determine if the device needs reprogramming or replacing. It can
also determine if another therapy, such as medication, is needed to manage a
heart rhythm disorder.
King Fahd Armed Forces Hospital,
Jeddah offers a new type of pacemaker called a leadless pacemaker. The
generator and a small wire are included in the 2-centimeter device, which is
implanted directly into the heart via a catheter through a vein.
Biventricular Pacemaker
A biventricular pacemaker works
like a conventional pacemaker, but uses a third wire to send electrical
impulses to the heart to resynchronize the contractions of the heart’s left
lower chamber, or ventricle.
Also called a cardiac
resynchronization device, this type of pacemaker is implanted when medications
don’t relieve symptoms of heart failure, a condition in which the heart
does not pump a sufficient amount of blood to the body, and when the left
chamber does not beat in a coordinated manner. This causes both ventricles to
contract out of sync with one another. A resynchronization device coordinates
the contractions of the left ventricle. Patient with Left Bundle Branch Block
ECG morphology wil usually need this type of pacemaker. There is biventricular pacemaker
that incorporated with implantable loop recorder as patient with heart failure
tend to get tachyarrhytmias such as ventricular tachycardia and ventricular
fibrillation.
Doctors provide local anesthesia
and a sedative when implanting a biventricular pacemaker. The surgery takes
about two hours to complete and requires an overnight stay in the hospital. The
restrictions afterward are the same as those recommended after the implantation
of a conventional pacemaker.
Your doctor electronically
monitors a biventricular pacemaker in the same way as a conventional pacemaker.
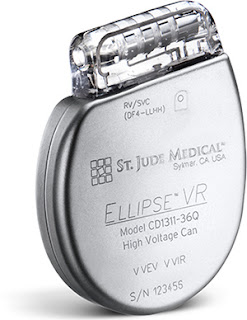
Implantable Cardioverter
Defibrillator
People with heart failure are
often at risk for life threatening, fast, irregular heartbeats called
ventricular arrhythmias. These people may need a combination biventricular
pacemaker and implantable cardioverter defibrillator, or ICD, which shocks the
heart’s rhythm back to normal.
Ventricular arrhythmia occurs
when irregular heartbeats originate in the heart’s ventricles, the lower
chambers that pump blood to the body. When this happens, the heart stops
pumping blood. If the rhythm is not corrected quickly, the result is sudden cardiac
arrest, a short-circuiting of the electrical signals that control the heart’s
ability to pump blood.
The heart usually pumps out about
60 percent of its blood with each beat, a measurement called ejection fraction.
When the heart’s ejection fraction is reduced to 35 percent or less, a person’s
risk for sudden cardiac arrest increases. If the reduced ejection fraction is
not caused by a condition that can be treated and reversed, surgeons often
implant an ICD.
In emergency situations, someone
can deliver a shock from an external defibrillator, if one is available, to
restore the heart to a normal rhythm. An ICD, however, detects an irregular
heartbeat and automatically and internally delivers a series of pacing pulses
or an electrical shock to the heart to correct the heart’s rate and rhythm.
An ICD stores information about
when and how many electrical shocks are delivered to the heart, whether they
corrected the arrhythmia, and the status of the device’s battery. Many ICDs
have a built-in pacemaker, which sends electrical impulses to the heart when it
is beating too slowly, helping it to beat at a normal rate.
People usually don’t notice small
pacing impulses that correct a fast heart rate (Anti Tachycardia Pacing-ATP),
but they do feel an uncomfortable “thump” in the chest when a shock is
delivered. If you notice one of these shocks, contact your doctor.
The ICD device is surgically
implanted in the chest wall below the collarbone. Surgery typically takes about
an hour and requires an overnight stay in the hospital. Your doctor may restrict
your activity, including driving and lifting items heavier than 10 pounds,
until your follow-up appointment 2 weeks after surgery.
If you are at risk of fainting
from a fast or irregular heart rhythm, driving may be restricted for longer
periods of time or permanently. Your heart condition, not the implanted device,
is the reason for this restriction.
The battery for an ICD typically
lasts 5 to 10 years.
A new type of defibrillator,
called a subcutaneous internal cardioverter defibrillator, is also offered in
our hospital. This device does not need to be implanted within the heart or a
blood vessel. The leads are implanted subcutaneously, or under the skin, which
helps to avoid complications associated with the implantation of a device in a
blood vessel.
Implantable Cardiac Loop
Recorder
Your cardiac electrophysiologist
may recommend surgically implanting a wireless cardiac monitor called a loop
recorder, which continuously records your heart’s rhythm for up to three years.
Smaller than the size of an AAA battery, this device is surgically inserted
beneath the skin of the upper chest to record the heart’s electrical activity,
much like an electrocardiogram, or EKG.
People who have had unexplained
fainting spells or heart palpitations that can’t be detected by short term
heart rhythm recording devices, such as Holter monitors, Rhythm card, King of
heart, may be candidates for this device. Doctors may also recommend an
implantable loop recorder for people with atrial fibrillation, which
causes a rapid and irregular heartbeat. In addition, this device is used in
people who have had a stroke for which a cause has not been
determined.
Your doctor makes a small
incision in the upper chest and inserts the device just under the skin. The
surgery is brief, and you can return to your usual activities the next day.
Your doctor may limit your activity until the incision heals.
Cardiac loop recorders typically
monitor the heart’s electrical activity for up to 36 months before replacement
is required. The device is removed through the original incision site through a
short surgery that is similar to the implantation procedure.
If you experience a fainting spell
or heart palpitations while this device is implanted in the chest, you or
another person places a handheld recorder over the device to capture and record
the heart’s electrical activity. This information is stored in the device and
can be transmitted via a remote monitoring system to help your doctor determine
the cause of your symptoms. The loop recorder is also able to automatically
record irregular heart rhythms.
The newest implantable cardiac
loop recorder is extremely small and can be injected under the skin. In this
procedure, a small puncture is made in the skin to the left of the breastbone.
The loop recorder is loaded into a small plastic applicator, which your doctor
uses to push the device under the skin. Dissolvable sutures are used to close the
small puncture. This procedure is performed with local anesthesia, and you can
go home afterwards.




















your blog is very interesting but if u want to learn any thing about a Herbal heart treatments or Heart Medicine then click here!
ReplyDelete